- School of Nursing and Midwifery, Shiraz University of Medical Sciences, Shiraz, Iran
Purpose: Considering effects of COVID-19 pandemic on the physical and mental health and professional quality of life (PQoL) of nurses working at COVID-19 wards, it seems necessary to investigate the factors affecting adaptation and reducing adverse effects of this pandemic on nurses. The present study aims to investigate the relationship between religious coping with post-traumatic stress disorder (PTSD) and professional quality of life (PQoL) among nurses.
Materials and methods: This descriptive correlational study was conducted on 368 nurses working at hospitals affiliated to Shiraz University of Medical Sciences. In this research, Mississippi scale for post-traumatic stress disorder (M-PTSD), Pargament’s brief religious coping measure (B-RCOPE) and Stamm’s professional quality of life (proQol) were used for data collection. Statistical significance was considered at p < 0.05.
Results: The mean score of positive religious coping was 13.01 ± 5.22 (moderate) and the mean score of negative religious coping was 5.27 ± 4.57 (low). The mean PTSD score of nurses was 96.92 ± 18.17 and most of them were at the moderate level (92.9%). The scores of compassion fatigue, secondary traumatic stress, and compassion satisfaction were in the moderate range. The Spearman’s correlation test results showed a significant and negative correlation between positive religious coping and PTSD, and a significant and positive correlation between negative religious coping and PTSD (p = 0.000). Moreover, a significant and positive correlation was observed between compassion satisfaction and positive religious coping (p = 0.005), and a negative and significant correlation was found between compassion fatigue and secondary stress and positive religious coping (p < 0.05). The statistical test of multiple regression revealed a significant correlation between nurses’ positive religious coping and compassion satisfaction, as well as between nurses’ negative religious coping and secondary stress and PTSD (p < 0.05).
Conclusion: Positive religious coping was correlated with reduced PTSD and improved PQoL among nurses.
Introduction
COVID-19 was first reported in Wuhan, China (December, 2019) and rapidly spread in whole China and, subsequently, worldwide (1, 2). The outbreak of this pandemic exposed the healthcare workers, as the frontline group, to the risk of physical and mental disorders (3). Although healthcare providers were also exposed to stress, compassion fatigue, depression, drug addiction and suicide before COVID-19 pandemic (4), initial world reports have revealed the incidence of depression, anxiety, Post-traumatic stress disorder (PTSD), suicide, compassion fatigue and sleep disorders increased among them after this pandemic (5–7). PTSD is among the psychological disorders among nurses that has been addressed by various studies during the pandemic period (8–12).
PTSD is considered a mental disorder that develops when an unfortunate and traumatic event threatens one’s life (13). Currently, PTSD is a growing concern in the nursing profession. Nurses are exposed to this disorder due to being either directly or indirectly in traumatic conditions and being responsible for taking care of patients (14).
Studies have demonstrated professional quality of life (PQoL) of healthcare providers decreased during COVID-19 pandemic (15, 16). PQoL is a multidimensional concept, consisting of two components of compassion satisfaction and compassion fatigue. The second component itself includes two components of compassion fatigue and secondary traumatic stress (17). Among all health-related professions, nurses are more prone to burnout, compassion fatigue and reduced job satisfaction due to the mental and physical stress caused by taking caring of critically ill patients (18). This issue is of particular importance because nurses’ PQoL is associated with the quality of nursing care, work productivity, burnout, job satisfaction, inappropriate performance, inappropriate violence, organizational effectiveness and organizational commitment (19–21). Currently, there is strong evidence on the inverse correlation between occupational stress and PTSD among nursing staff as well as between their perceived job satisfaction and PQoOL (22–24).
Secondary traumatic stress is considered a negative aspect in PQoL, which plays a vital role in nurses’ physical and mental health (25). During stressful events, coping strategies are stabilizing methods used to help individuals maintain psychological adaptation (26). Coping strategies could be defined as cognitive and behavioral measures used to manage stressful conditions (27). Coping strategies affect one’s feelings or thoughts to create a good quality of life and make a positive action (28). Adopting an appropriate coping strategy plays a major role in relieving PTSD symptoms (29). However, coping strategies could cause severe psychological stress, if not appropriately used (28).
Spirituality has received great attention as an important coping strategy for promoting psychological well-being among patients and healthcare workers (30). Religion is often considered an important and well-known aspect of spirituality (31). Religious coping is defined as using religious beliefs and behaviors to solve problems and prevent or relieve negative psychological consequences when faced with difficult problems and conditions (32).
Religious coping includes two positive and negative dimensions. Positive religious coping (PRC) involves ways of facing negative life events, in which one accepts the events using positive appraisals and interpretations related to God’s will. However, in other form of coping, called negative religious coping (NRC), a person establishes an avoidant and insecure relationship with God. PRC involves benefiting from a favorable connection with God or higher power during the crisis. In NRC, one blames God for their difficulties. Positive and negative religious coping is associated with higher and lower levels of psychological health, respectively (33). Studies have reported positive religious coping during infectious disease outbreaks could help individuals reduce the risk of depression (34, 35). However, some studies have not found a significant correlation between positive religious coping and lower levels of anxiety, depression and concern (36–39). The conflicting results show the necessity of conducting further studies in this field.
Considering the effect of COVID-19 pandemic on the physical and mental health and PQoL of nurses working at COVID-19 wards, it seems necessary to investigate the factors affecting adaptation and reducing adverse effects of this pandemic on nurses as their adaptation could be improved by identifying and strengthening these factors. Although the relationship between religious coping and some variables has been previously investigated separately, these variables have been less addressed during COVID-19 pandemic, which imposed a severe and chronic stress on nurses. The aim of the present study was to investigate the corellations between religious coping with PTSD and PQoL of nurses working at COVID-19 wards.
Some studies have been conducted separately on nurses’ post-traumatic stress disorder, quality of professional life, and religious adjustment and coping strategies during the COVID-19 pandemic (40–47). Studies on the relationship between religious coping and post-traumatic stress disorder have been limited and show contradictory results (38, 48, 49). However we could not find any study which investigated the multivariate relationship between all three mentioned variables. This gap in studies indicates the necessity of conducting the present study which aimed to investigate the correllations between religious coping with PTSD and PQoL of nurses working at COVID-19 wards.
Materials and methods
Study type and setting
In this descriptive correlational study, the nurses working at COVID-19 wards of five hospitals affiliated to Shiraz University of Medical Sciences, southern Iran, during the last 6 months.
Sampling and sample size
Participants were selected using convenience sampling method. The sample size was determined 304 individuals based on the results of a similar study (50) using G*Power software considering the power of 80% and α = 0.05, which increased to 365, taking into account the withdrawal rate of 20%.
The inclusion criteria were having at least a bachelor’s degree in nursing, having at least 2 months of work experience at COVID-19 wards at the time of completing the questionnaire, not suffering from known mental illnesses such as anxiety and severe depression, not facing physical or mental traumatic events within 6 months before the study, lack of severe work or communication problems in the workplace (The last three items were based on the participants’ self-report) and being willing to participate in the study. The exclusion criterion was failure to complete the questionnaires.
Measurements
In this study, demographic questionnaire (including age, gender, level of education, marital status, total work experience, length of time working in the COVID-19 wards, living with high-risk people, and how religious they are from their point of view), Mississippi scale for post-traumatic stress disorder (M-PTSD), Pargament’s brief religious coping measure (B-RCOPE) and Stamm’s professional quality of life (proQol) were used to collect data.
The self-report 39-item M-PTSD was developed and introduced by Norris and Raid (99). The items with a star are scored based on a 5-point Likert scale, ranging from (5) very often true to (1) never true, and items without a star are reverse-scored, and the total score ranges between 0 and 195. Scores less than 65, 65–130 and above 130 are considered mild, moderate and severe, respectively (51). The Cronbach’s alpha coefficient of this scale was reported as 0.86–0.94 (52). In the present study, the Persian version of this scale, which has been previously used in various studies in Iran and its validity and reliability have been confirmed, was employed (51–54). This scale was validated by Goodarzi (51) in Iran. The scale reliability was obtained as 0.92, 0.92, 0.91, and 0.82 based on the internal consistency, split-half method, test–retest method and peer test (PTSD inventory) (53). In the present study, Cronbach’s alpha for the M-PTSD questionnaire was determined to be 0.88.
The 14-item brief religious coping measure (B-RCOPE) was developed by Pargament (100). In this questionnaire, each of the positive and negative scales includes 7 items. Items 1–7 indicate positive religious coping and items 8–14 indicate negative religious coping. The items are scored based on a 4-point Likert scale, ranging from “never” to “always” (0–3). The minimum and maximum scores of each subscale of positive and negative religious coping are 0 and 21, respectively. The religious orientation scale (ROS) was used as a reference to assess the reliability and validity of the Persian version of this scale in a preliminary study conducted in 2001. Concurrent validity was assessed using religious coping scale. The correlation between the scores obtained from the simultaneous use of the two scales was obtained as 0.6 (101, 102). Cronbach’s alpha coefficient was calculated to evaluate the scale validity. This coefficient was obtained as 0.86 and 0.65 in the subscales of positive and negative religious coping, respectively (55). In this study, the values of Cronbach’s alpha coefficient were obtained as 0.90 and 0.83 for positive and negative religious coping, respectivelyThe self-report 30-item professional quality of life (proQol) was designed and developed by Stamm. This scale includes three dimensions of compassion satisfaction (items 3, 6, 12, 16, 18, 20, 22, 24, 27, 30), compassion fatigue (items 1, 4, 8, 15, 10, 17, 19, 21, 26, 29) and secondary traumatic stress (items 2, 5, 7, 9, 11, 13, 14, 23, 25, 28). Each dimension consists of 10 items scored based on a 5-point Likert scale (1 = never to 5 = very often). The score of each subscale is obtained from the sum of all its items, so that the score of each subscale varies between 10 and 50. Each subscale consists of 10 items. In all the three subscales, the score of 22 or less indicates low level of compassion satisfaction, compassion fatigue and secondary traumatic stress, the score of 23–41 indicates moderate level of compassion satisfaction, compassion fatigue and secondary traumatic stress, and the score of 42 and higher indicates high level of compassion satisfaction, compassion fatigue and secondary traumatic stress (56). In the present study, the Persian version of this scale, which has been previously used in various studies in Iran and its validity and reliability have been confirmed, was employed. The validity and reliability of the whole scale was confirmed in the study by Yadollahi et al. and its Cronbach’s alpha was reported as 0.70 (57). In other studies, the alpha coefficient was reported as 0.73 and 0.75 (58, 59). In the present study, the Cronbach coefficient was estimated as 0.88, 0.74, 0.84, and 0.65 for compassion satisfaction, compassion fatigue, secondary traumatic stress, and proQol total use score, respectively.
Data collection
The samples were first selected using the convenience sampling method considering the inclusion criteria. After explaining the research objectives and methodology, the participants signed the informed consent form. The questionnaires were given and collected by researcher (first author) and her assistant and collected after completing. Due to the multiplicity of questionnaires and the large number of questions and in order to maintain the cooperation of the samples, the questionnaires were collected 2 days after distribution. In total, 375 questionnaires were completed, 7 of which were excluded due to high missing values, and the data of 368 nurses were analyzed.
Statistical analysis
The data were analyzed using SPSS 26.0. Given that the data were not normally distributed, non-parametric Mann–Whitney and Kruskal-Wallis tests were used. Pearson’s correlation coefficient and its non-parametric equivalent, i.e., Spearman’s correlation, as well as multiple regression were employed to investigate the correlation between the quantitative variables. p-value < 0.05 was considered statistically significant.
Ethical considerations
This study was approved by Research Ethics Committee of Shiraz University of Medical Sciences (No: IR.SUMS.NUMING.REC.1401.30). All the participants signed the informed consent form after receiving information about research objectives and methodology. The participants were assured that their information would be kept confidential and anonymous. It was emphasized that it would not have any impact on their professional status if they do not participate or withdrawal from the study.
Results
The mean age of the nurses participating in the study was 31.43 ± 6.45 years old, ranging from 22 to 55 years old. The mean work experience of nurses was 8.21 ± 6.44, ranging from 6 months to 28 years, and the mean work experience at the COVID-19 ward was 16.11 ± 10.91, ranging from 2 to 36 months. Most of the nurses were female (77.40%) and married (54%) and had a bachelor’s degree (90%). The majority of the nurses were working at non-intensive units (61%) and did not live with older adult people (61.5%) or those with chronic diseases (85.50%). Most of them considered themselves to be moderately religious (54%) (Table 1).
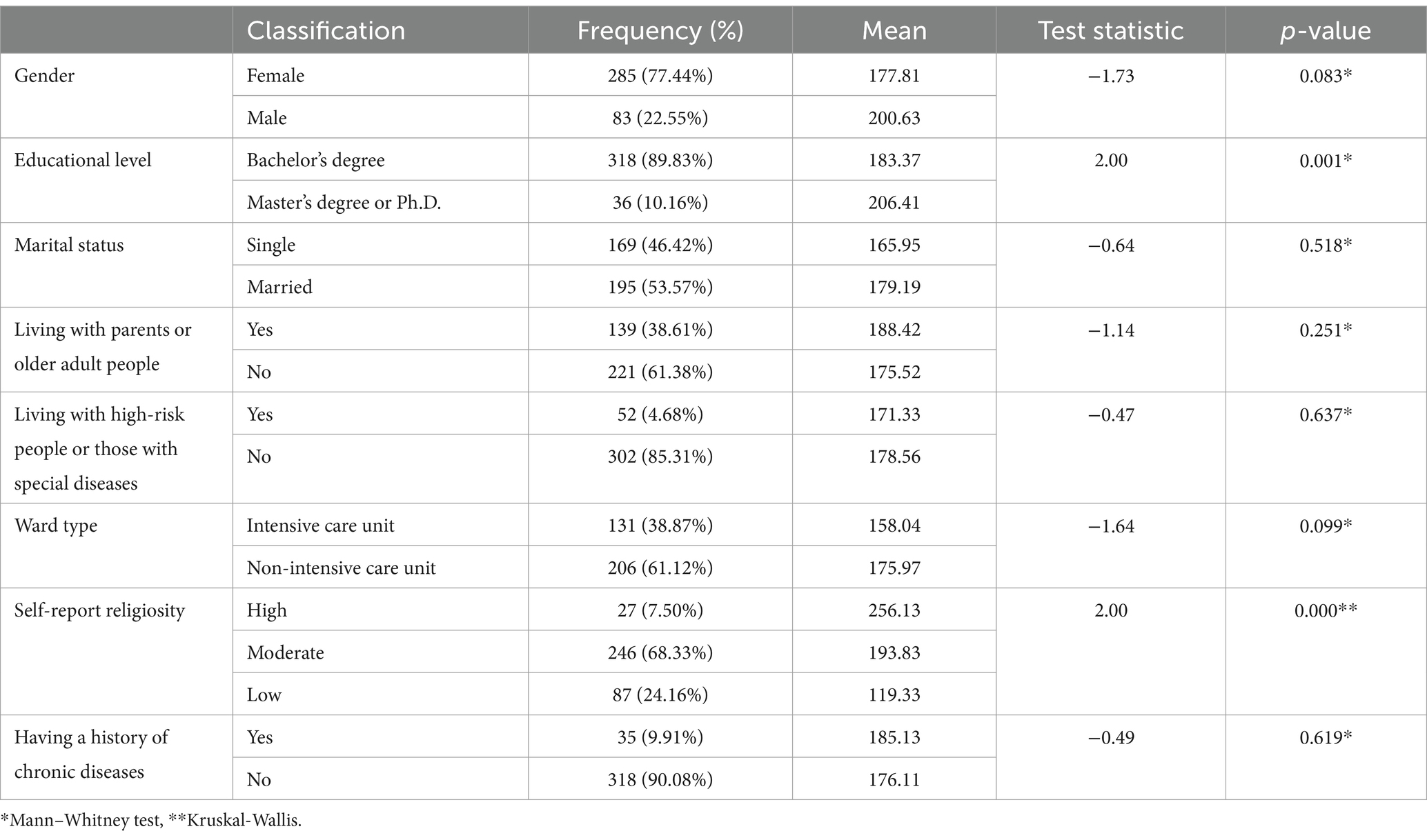
Table 1. Mean score of religious coping considering demographic characteristics of nurses working at COVID-19 ward.
The mean score of positive religious comping was 13.01 ± 5.22, which was at the moderate level. Also, the mean score of negative religious coping was 4.57 ± 5.27, which was at the low level. A significant correlation was observed between religious coping and educational level (p = 0.03) and rself-report eligiosity (p = 0.000).
Figure 1 presents the mean and standard deviation of PQoL and PTSD scores.
The Spearman’s correlation test results showed a significant, negative correlation between positive religious coping and PTSD and a significant positive correlation between negative religious coping and PTSD (p < 0.05). PTSD had a stronger correlation with negative religious coping (r = 0.485) (Table 2). The Spearman’s correlation test results showed a positive significant correlation between compassion satisfaction and positive religious coping (p = 0.005) and a significant, negative correlation between compassion fatigue and secondary stress and positive religious coping (p < 0.05). There was a significant and adverse correlation between negative religious coping and compassion satisfaction, and a positive and significant correlation between compassion fatigue and secondary stress (p < 0.05) (Table 2).
The statistical test of multiple regression revealed a significant correlation between positive religious coping and compassion satisfaction among nurses (p < 0.05). If considering PTSD constant and adding one point to the positive religious coping score, 0.375 point will be added to the compassion satisfaction score. No significant correlation was found between positive religious coping and PTSD (p = 0.289). Also, no significant correlation was observed between compassion fatigue, secondary stress, PTSD and positive religious coping (p > 0.05) (Table 3).
The statistical test of multiple regression revealed a significant correlation between negative religious coping and secondary stress and PTSD among nurses (p = 0.000). If considering PTSD constant and adding one point to the negative religious coping score, 0.294 point will be added to the secondary stress score. If considering secondary stress constant and adding one point to the negative religious coping score, 0.247 point will be added to the PTSD score. However, no significant correlation was found between compassion fatigue, compassion satisfaction and negative religious coping (p > 0.05) (Table 4).
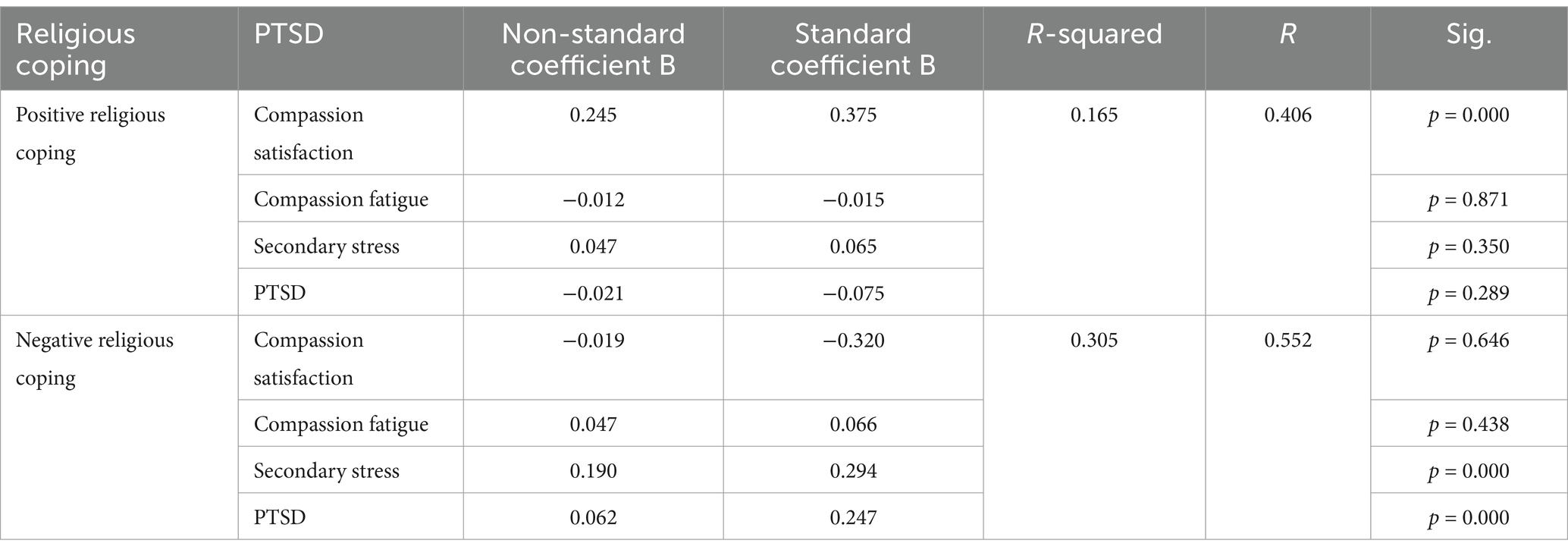
Table 4. Multivariate correlation between compassion satisfaction, compassion fatigue, secondary stress and PTSD with positive and negative religious coping.
Discussion and conclusion
Results of the present study showed the mean scores of positive and negative religious coping were at the moderate and low levels, respectively, and positive religious coping had a higher mean score than negative religious coping. In studies by Ken Chow et al. and Francis et al. on healthcare workers working in a hospital during COVID-19 pandemic in Malaysia, the mean score of positive and negative religious coping was greater than the study present. However, the mean positive religious coping score was higher than the negative religious coping score, which was in line with the present study (41, 60). In some other studies conducted in Asian countries, positive religious coping was used more than negative religious coping (61, 62). It seems that healthcare workers tend to rely more on God or supreme existence under critical conditions (63). Not surprisingly, participants with greater self-report religiosity were significantly more likely to use religious coping. Religious coping was, in turn, associated with greater mental health, in line with previous research (64–67). The results showed significant correlation between religious coping and educational level. Although in one study there was no correlation between education level and religious coping (68), in some another studies educational level was directly correlated with spiritual experiences and religious coping (69, 70). These difference may stem from participants charactristics and cultural background.
In the present study, more than 90% of the nurses working at COVID-19 wards had moderate PTSD. Various studies have confirmed the increased incidence of PTSD at moderate and severe levels among healthcare providers and nurses working at COVID-19 wards (71–73).
In studies by Almeida and Mirab Zadeh Ardekani, the mean PTSD score has been at the severe level among about half of the participants, and the risk of suffering from PTSD in Almeida’s study was higher than that of the present study. It seems that these investigations were carried out during the COVID-19 pandemic in the absence of sufficient protective facilities when there was difficulty in controlling the disease, which brought more stress (8, 74).
The scores of all the three dimensions of PQoL scale, including compassion satisfaction, compassion fatigue and secondary stress, were at the moderate level, and compassion satisfaction had a higher mean score. Various studies conducted during the COVID-19 pandemic in the United States, as well as studies by Carla Serrão and Cuartero-Castañer in Portugal and Ecuador have shown the moderate level of compassion fatigue and secondary traumatic stress and moderate to high levels of compassion satisfaction (75–77). However, another research indicated most of the healthcare professionals had high levels of compassion fatigue and moderate to high levels of burnout and compassion satisfaction (78). Trumello et al. found that those working in areas with higher likelihood of disease transmission reported a higher level of compassion fatigue and a lower level of compassion satisfaction (79).
The conflicting results could be due to the point that these studies were mainly conducted in the initial peaks of COVID-19, while more adaptation was achieved over time using coping strategies. On the other hand, the present study was conducted after vaccination against COVID-19, which could affect the stress level and, as a result, nurses’ PQoL (80).
This study showed PTSD was significantly and inversely correlated with positive religious coping, and there was a relatively strong positive correlation between PTSD and negative religious coping. Moreover, there was a negative and significant correlation between intrusive memories, difficulty in interpersonal communication, inability to control emotions and positive religious coping. Also, a significant and positive correlation was observed between intrusive memories, difficulty in interpersonal communication, inability to control emotions, loss and depression and negative religious coping. In general, PTSD had a stronger correlation with negative religious coping, and the total religious coping score had the maximum correlation with intrusive memories and minimum correlation with inability to control emotions.
Studies by Reiner Fuentes-Ferrada and Tatum Feiler demonstrated negative religious coping was among the risk factors for PTSD among students, which was in line with results of our study (35, 81). Investigations have revealed respondents who used positive religious coping showed less PTSD symptoms than those who used negative religious coping (82–84).
There was a significant, positive correlation between compassion satisfaction and positive religious coping and a negative and significant correlation between compassion fatigue and secondary stress and positive religious coping. A significant and negative correlation was found between negative religious coping and compassion satisfaction. However, a significant and positive correlation was observed between negative religious coping and compassion fatigue and secondary stress.
Moreover, there is a significant correlation between nurses’ PQoL and religious coping. Nurses’ PQoL could be improved by promoting the quality of religious coping because religious people with high spirituality experience higher compassion satisfaction and lower compassion fatigue and burnout (85–87). It seems that people see themselves connected to a source of energy by taking advantage of religious beliefs and deal with burnout and fatigue with more tolerance using better coping strategies (56). This issue is more tangible in Iran, which has a religious background (88).
In this study, all PTSD dimensions were significantly and negatively correlated with compassion satisfaction, and all PTSD dimensions were significantly and positively correlated with compassion fatigue. Also, all PTSD dimensions were significantly and positively correlated with secondary stress. The strongest correlation was observed between intrusive memories and compassion fatigue. Some other studies have confirmed these findings (89–91).
Results of this study indicated positive religious coping had a greater impact on the compassion satisfaction than PTSD. Also, negative religious coping affected the secondary stress and PTSD, and negative religious coping had a greater effect on the secondary stress. Studies have revealed improving the quality of positive religious coping could increase nurses’ QOL (85) and positive religious coping strategies have been associated with promoting well-being and personal growth (92). Religiosity and spirituality are resources that provide a coping strategy for mental disorders, especially under stressful conditions (93). Various studies have shown negative religious coping is associated with increased psychological complications and disorders, secondary stress and post-traumatic stress (60, 82, 83, 94). Also some recent works on religious coping and mental health wellbeing among healthcare workers, found that healthcare workers employed more positive than negative coping strategies when dealing with their struggles (60, 61, 95). It seems that the positive religious coping is associated with better physical and mental health outcomes (96). Research has shown benefits of positive religious coping on mental health and opposite results of negative religious coping in different populations (97, 98).
Conclusion
The results showed religious coping could affect nurses’ PQoL and PTSD working at COVID-19 wards. Positive religious coping was correlated negatively with PTSD and positively with PQoL. PTSD had a stronger correlation with negative religious coping.
The effect of COVID-19 pandemic on nurses’ physical and mental health and PQOL working at COVID-19 wards, which may continue for years, demonstrates the necessity of reducing the negative effects of this pandemic on nurses. Training and using different strategies to strengthen effective coping, especially religious coping, could be considered to better adapt nurses to the effects of the pandemic crisis. Holding educational workshops and in-service classes could affect nurses’ performance and viewpoints in this regard. Moreover, specialized psychological and religious counseling is recommended for nurses with high stress levels and negative religious coping users.
Although multicenter designing is the strength of this study which enhances the generalizability of the results, conducting it in a specific cultural background may limit the generalizability of the findings to other regions or healthcare settings. Another limitation of this study was that high workload and fatigue of nurses working in the hospital may have affected their responses, which could not be controlled. Furthermore, the data collection through self-report measures, may have affected accuracy of the data.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Author contributions
ZS: Conceptualization, Methodology, Software, Formal analysis, Investigation, Resources, Data curation, Project administration, Funding acquisition, Writing – original draft. PT: Conceptualization, Methodology, Formal analysis, Investigation, Writing – review & editing. MM: Conceptualization, Methodology, Software, Validation, Formal analysis, Investigation, Visualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was extracted from the M.Sc. thesis of Zohreh Sanavi Shiri in Medical-Surgical nursing, and was approved and financially supported by Shiraz University of Medical Sciences (no. 25804). The funder had no role in the design of the study, nor in the collection, analysis, and interpretation of the data and in writing the manuscript.
Acknowledgments
We would like to thank Vice-Chancellor for Research of Shiraz University of Medical Sciences and directors of Namazi, Faqihi, Rajaei, Chamran and Ali-Asghar hospitals and all the participants in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
PQOoL, professional quality of life; PTSD, post-traumatic stress disorder; M-PTSD, post-traumatic stress disorder; B-RCOPE, brief religious coping measure; PRC, Positive religious coping; NRC, negative religious coping.
References
1. Bansal, N, and Ghafur, A. COVID-19 in oncology settings. Cancer Res Stat Treat. (2020) 3:13–S4. doi: 10.4103/CRST.CRST_92_20
2. Haghbin, M, Abbasi, A, Rafei, E, Kheradmand, A, Javdani, F, Hatami, N, et al. Anxiety caused by new coronavirus (Covid-19) in breast cancer patients during the coronavirus pandemic. Iran J Obstetr Gynecol Infertil. (2020) 23:8–17. doi: 10.22038/IJOGI.2020.17286
3. Greene, T, Harju-Seppänen, J, Adeniji, M, Steel, C, Grey, N, Brewin, CR, et al. Predictors and rates of PTSD, depression and anxiety in UK frontline health and social care workers during COVID-19. Eur J Psychotraumatol. (2021) 12:1882781. doi: 10.1080/20008198.2021.1882781
4. Carrieri, D, Briscoe, S, Jackson, M, Mattick, K, Papoutsi, C, Pearson, M, et al. ‘Care under pressure’: a realist review of interventions to tackle doctors’ mental ill-health and its impacts on the clinical workforce and patient care. BMJ Open. (2018) 8:e021273. doi: 10.1136/bmjopen-2017-021273
5. Gunnell, D, Appleby, L, Arensman, E, Hawton, K, John, A, Kapur, N, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. (2020) 7:468–71. doi: 10.1016/S2215-0366(20)30171-1
6. Lai, J, Ma, S, Wang, Y, Cai, Z, Hu, J, Wei, N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
7. Rossi, R, Socci, V, Pacitti, F, Di Lorenzo, G, Di Marco, A, Siracusano, A, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. (2020) 3:e2010185. doi: 10.1001/jamanetworkopen.2020.10185
8. Ardekani, BMZ, Boroujerdi, FG, Dolabinjad, SE, Safa, M, and Zadeh, FH. Depression, anxiety, stress, and post-traumatic stress disorder among Iranian nursing caring for COVID-19 patients. Human Indonesian Psychol J. (2023) 20:69–79. doi: 10.26555/humanitas.v20i1.270
9. Biber, J, Ranes, B, Lawrence, S, Malpani, V, Trinh, TT, Cyders, A, et al. Mental health impact on healthcare workers due to the COVID-19 pandemic: A US cross-sectional survey study. J Patient Rep Outcomes. (2022) 6:63. doi: 10.1186/s41687-022-00467-6
10. Sahin, MK, Aker, S, Şahin, G, and Karabekiroğlu, A. Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 pandemic in Turkey. J. Community Health. (2020). 45:1168–77. doi: 10.1007/s10900-020-00921-w
11. Koohsari, E, Darban, F, Safarzai, E, and Kordi, M. Understanding the effect of post-traumatic stress on the professional quality of life of pre-hospital emergency staff. Emerg Nurse. (2021) 29:33–40. doi: 10.7748/en.2021.e2073
12. Van Wert, MJ, Gandhi, S, Gupta, I, Singh, A, Eid, SM, Haroon Burhanullah, M, et al. Healthcare worker mental health after the initial peak of the COVID-19 pandemic: a US medical center cross-sectional survey. J Gen Intern Med. (2022) 37:1169–76. doi: 10.1007/s11606-021-07251-0
13. American Psychiatric Association. The American Psychiatric Association Practice Guideline for the Treatment of Patients with Schizophrenia. Washington, DC: American Psychiatric Association Publishing (2020).
14. Schuster, M, and Dwyer, PA. Post-traumatic stress disorder in nurses: an integrative review. J Clin Nurs. (2020) 29:2769–87. doi: 10.1111/jocn.15288
15. Amdal, CD, Taylor, K, Kuliś, D, Falk, RS, Bottomley, A, Arraras, JI, et al. Health-related quality of life in patients with COVID-19; international development of a patient-reported outcome measure. J Patient Rep Outcomes. (2022) 6:26. doi: 10.1186/s41687-022-00434-1
16. Huang, F, Yang, Z, Wang, Y, Zhang, W, Lin, Y, Zeng, L-c, et al. Health-related quality of life and influencing factors of pediatric medical staff during the COVID-19 outbreak. Front Public Health. (2020) 8:565849. doi: 10.3389/fpubh.2020.565849
17. Magnavita, N, Soave, PM, Ricciardi, W, and Antonelli, M. Occupational stress and mental health among anesthetists during the COVID-19 pandemic. Int J Environ Res Public Health. (2020) 17:8245. doi: 10.3390/ijerph17218245
18. Kim, K, Han, Y, and Kim, J-s. Korean nurses’ ethical dilemmas, professional values and professional quality of life. Nurs Ethics. (2015) 22:467–78. doi: 10.1177/0969733014538892
19. Akter, N, Akkadechanunt, T, Chontawan, R, and Klunklin, A. Factors predicting quality of work life among nurses in tertiary-level hospitals, Bangladesh. Int Nurs Rev. (2018) 65:182–9. doi: 10.1111/inr.12401
20. Eren, H, and Hisar, F. Quality of work life perceived by nurses and their organizational commitment level. J Hum Sci. (2016) 13:1123–32. doi: 10.14687/ijhs.v13i1.3440
21. Prasad, M. An evaluation of the quality of work life: a study of the public sector nurses in West Bengal. Asian J Nurs Educ Res. (2016) 6:199–203. doi: 10.5958/2349-2996.2016.00036.7
22. Ghawadra, SF, Abdullah, KL, Choo, WY, and Phang, CK. Psychological distress and its association with job satisfaction among nurses in a teaching hospital. J Clin Nurs. (2019) 28:4087–97. doi: 10.1111/jocn.14993
23. Lee, J-H, Hwang, J, and Lee, K-S. Job satisfaction and job-related stress among nurses: the moderating effect of mindfulness. Work. (2019) 62:87–95. doi: 10.3233/WOR-182843
24. Soto-Rubio, A, Giménez-Espert, MDC, and Prado-Gascó, V. Effect of emotional intelligence and psychosocial risks on burnout, job satisfaction, and nurses’ health during the covid-19 pandemic. Int J Environ Res Public Health. (2020) 17:7998. doi: 10.3390/ijerph17217998
25. Fu, CY, Yang, MS, Leung, W, Liu, YY, Huang, HW, and Wang, RH. Associations of professional quality of life and social support with health in clinical nurses. J Nurs Manag. (2018) 26:172–9. doi: 10.1111/jonm.12530
26. Mariani, R, Renzi, A, Di Trani, M, Trabucchi, G, Danskin, K, and Tambelli, R. The impact of coping strategies and perceived family support on depressive and anxious symptomatology during the coronavirus pandemic (COVID-19) lockdown. Front Psych. (2020) 11:587724. doi: 10.3389/fpsyt.2020.587724
27. Ramos, FP, Enumo, SRF, and Paula, KMP. Motivational theory of coping: a developmental proposal for the analysis of coping with stress. Estudos de Psicologia (Campinas). (2015) 32:269–79. doi: 10.1590/0103-166X2015000200011
28. Mashudi, S, and Yusuf, A. Family coping strategies to improve the health of family members living with schizophrenia. Jurnal Ners. (2021) 16:67–73. doi: 10.20473/jn.v16i1.24527
29. Wang, Y-X, Guo, H-T, Du, X-W, Song, W, Lu, C, and Hao, W-N. Factors associated with post-traumatic stress disorder of nurses exposed to corona virus disease 2019 in China. Medicine. (2020) 99:e20965. doi: 10.1097/MD.0000000000020965
30. Roman, NV, Mthembu, TG, and Hoosen, M. Spiritual care–‘A deeper immunity’–A response to Covid-19 pandemic. Afric J Primary Health Care Fam Med. (2020) 12:1–3. doi: 10.4102/phcfm.v12i1.2456
31. Moreira-Almeida, A, Sharma, A, Van Rensburg, BJ, Verhagen, PJ, and Cook, CC. WPA position statement on spirituality and religion in psychiatry. Actas espanolas de psiquiatria. (2018) 46:242–8.
32. Matthews, DA, McCullough, ME, Larson, DB, Koenig, HG, Swyers, JP, and Milano, MG. Religious commitment and health status: a review of the research and implications for family medicine. Arch Fam Med. (1998) 7:118–24. doi: 10.1001/archfami.7.2.118
33. Pargament, KI, Tarakeshwar, N, Ellison, CG, and Wulff, KM. Religious coping among the religious: the relationships between religious coping and well-being in a national sample of Presbyterian clergy, elders, and members. J Sci Study Relig. (2001) 40:497–513. doi: 10.1111/0021-8294.00073
34. Cheng, C, and Ying, W. A meta-analytic review of the associations between dimensions of religious coping and psychological symptoms during the first wave of the COVID-19 pandemic. Front Psych. (2023) 14:1097598. doi: 10.3389/fpsyt.2023.1097598
35. Fuentes-Ferrada, R, Cerda-Planas, C, and Fernández, MB. Religious coping, experiential avoidance, self-compassion, and post-traumatic stress by COVID-19: a serial mediation study. Int J Lat Am Relig. (2023) 7:562–73. doi: 10.1007/s41603-022-00184-4
36. Harris, JI, Leak, GK, Dubke, R, and Voecks, C. Religious strain and postconventional religiousness in trauma survivors. Psychol Relig Spiritual. (2015) 7:173–8. doi: 10.1037/rel0000026
37. Lupo, MK, and Strous, RD. Religiosity, anxiety and depression among Israeli medical students. Isr Med Assoc J. (2011) 13:613–8.
38. O'Brien, B, Shrestha, S, Stanley, MA, Pargament, KI, Cummings, J, Kunik, ME, et al. Positive and negative religious coping as predictors of distress among minority older adults. Int J Geriatr Psychiatry. (2019) 34:54–9. doi: 10.1002/gps.4983
39. Thomas, J, and Barbato, M. Positive religious coping and mental health among Christians and Muslims in response to the COVID-19 pandemic. Religions. (2020) 11:498. doi: 10.3390/rel11100498
40. Bagheri Sheykhangafshe, F, Saeedi, M, Ansarifar, N, Savabi Niri, V, and Deldari, AM. Evaluation of post-traumatic stress disorder, depression and anxiety of nurses during coronavirus 2019 pandemic: a systematic review. Iran J Nurs Res. (2021) 16:58–70.
41. Francis, B, Ken, CS, Han, NY, Ariffin, MAA, Yusuf, MHM, Wen, LJ, et al. Religious coping during the COVID-19 pandemic: gender, occupational and socio-economic perspectives among Malaysian frontline healthcare workers. Alpha Psychiatry. (2021) 22:194–9. doi: 10.5152/alphapsychiatry.2021.21185
42. Habibi Soola, A, Mozaffari, N, and Mirzaei, A. Spiritual coping of emergency department nurses and emergency medical services staff during the COVID-19 pandemic in Iran: an exploratory study. J Relig Health. (2022) 61:1657–70. doi: 10.1007/s10943-022-01523-7
43. Esmaili, DNS., Safa, M, Ghasem, BF, Hajizadeh, F, and Mirabzadeh, AB. Incidence of post-traumatic stress disorder after covid-19 among medical staff of masih daneshvari hospital. J. Med. Counc. I.R.I. [Internet. (2020) 38:27–33. Available from: https://sid.ir/paper/381977/en
44. Sehularo, LA, Molato, BJ, Mokgaola, IO, and Gause, G. Coping strategies used by nurses during the COVID-19 pandemic: a narrative literature review. Health SA Gesondheid (Online). (2021) 26:1–8. doi: 10.4102/hsag.v26i0.1652
45. Sierakowska, M, and Doroszkiewicz, H. Stress coping strategies used by nurses during the COVID-19 pandemic. PeerJ. (2022) 10:e13288. doi: 10.7717/peerj.13288
46. Zakeri, MA, Ghaedi-Heidari, F, Khaloobagheri, E, Hossini Rafsanjanipoor, SM, Ganjeh, H, Pakdaman, H, et al. The relationship between nurse’s professional quality of life, mindfulness, and hardiness: a cross-sectional study during the COVID-19 outbreak. Front Psychol. (2022) 13:866038. doi: 10.3389/fpsyg.2022.866038
47. Zakeri, MA, Rahiminezhad, E, Salehi, F, Ganjeh, H, and Dehghan, M. Compassion satisfaction, compassion fatigue and hardiness among nurses: a comparison before and during the COVID-19 outbreak. Front Psychol. (2022) 12:815180. doi: 10.3389/fpsyg.2021.815180
48. Amiri, F, Asadi Noghbi, F, Yousefi, H, Makkizade, V, Madani, A, Aghamolaei, T, et al. Post-traumatic stress and its relationship with burnout in workers during COVID-19 pandemic. J Prev Med. (2021) 8:58–48. doi: 10.52547/jpm.8.2.58
49. Francis, B, Gill, JS, Yit Han, N, Petrus, CF, Azhar, FL, Ahmad Sabki, Z, et al. Religious coping, religiosity, depression and anxiety among medical students in a multi-religious setting. Int J Environ Res Public Health. (2019) 16:259. doi: 10.3390/ijerph16020259
50. Chavoshian, SA, Moeini, B, Bashirian, S, and Feradmal, J. The role of spiritual health and social support in predicting nurses’ quality of life. J Educ Commun Health. (2015) 2:19–28.
51. Goodarzi, MA. Evaluating validity and reliability of mississippi post-traumatic stress disorder scale. J. Psychol. [Internet]. (2003) 7:153–78. Available from: https://sid.ir/paper/54490/en
52. Keane, TM, Caddell, JM, and Taylor, KL. Mississippi scale for combat-related posttraumatic stress disorder: three studies in reliability and validity. J Consult Clin Psychol. (1988) 56:85–90. doi: 10.1037/0022-006X.56.1.85
53. Goodarzi, M. Evaluating reliability and validity of the Mississippi scale for post-traumatic stress disorder in shiraz. J Psychol. (2003) 7:153–78.
54. Mcfall, ME, Smith, DE, Mackay, PW, and Tarver, DJ. Reliability and validity of Mississippi scale for combat-related posttraumatic stress disorder. Psychol Assess. (1990) 2:114–21. doi: 10.1037/1040-3590.2.2.114
55. Hasany Wajari, K, and Bahrami Ehsan, H. Relationship between religious coping style and spiritual well-being. J. Psychol. [Internet]. (2005). 9:248–60. Available from: https://sid.ir/paper/371306/en
56. Boroomand Soleiman, SA, Salehi, S, and Abbasi, AN. The effect of spiritual care training on the professional quality of life of nurses in intensive care units. 2. J Nurs Educ. (2022) 11:24–35. doi: 10.22034/JNE.11.6.24
57. Yadollahi, M, Razmjooei, A, Jamali, K, Niakan, MH, and Ghahramani, Z. The relationship between professional quality of life (ProQol) and general health in Rajaee trauma hospital staff of shiraz. Iran Shiraz E Med J. (2016) 17:17. doi: 10.17795/semj39253
58. Nejad, N, Hosseini, M, Mirzaei, SM, and Moghaddam, Z. Association between resilience and professional quality of life among nurses working in intensive care units. Iran J Nurs. (2019) 31:49–60. doi: 10.29252/ijn.31.116.49
59. Vagharseyyedin, SA, Zarei, B, and Hosseini, M. The role of workplace social capital, compassion satisfaction and secondary traumatic stress in affective organisational commitment of a sample of Iranian nurses. J Res Nurs. (2018) 23:446–56. doi: 10.1177/1744987118762974
60. Chow, SK, Francis, B, Ng, YH, Naim, N, Beh, HC, Ariffin, MAA, et al. Religious coping, depression and anxiety among healthcare workers during the COVID-19 pandemic: a Malaysian perspective. Healthcare (Basel). (2021) 9:79. doi: 10.3390/healthcare9010079
61. Grover, S, Sarkar, S, Bhalla, A, Chakrabarti, S, and Avasthi, A. Religious coping among self-harm attempters brought to emergency setting in India. Asian J Psychiatr. (2016) 23:78–86. doi: 10.1016/j.ajp.2016.07.009
62. Nurasikin, MS, Khatijah, LA, Aini, A, Ramli, M, Aida, SA, Zainal, NZ, et al. Religiousness, religious coping methods and distress level among psychiatric patients in Malaysia. Int J Soc Psychiatry. (2013) 59:332–8. doi: 10.1177/0020764012437127
63. McKay, R, and Whitehouse, H. Religion and morality. Psychol Bull. (2015) 141:447–73. doi: 10.1037/a0038455
64. Koenig, HG. Religion, spirituality, and health: the research and clinical implications. ISRN Psychiatry. (2012) 2012:278730:1–33. doi: 10.5402/2012/278730
65. Magin, ZE, David, AB, Carney, LM, Park, CL, Gutierrez, IA, and George, LS. Belief in god and psychological distress: is it the belief or certainty of the belief? Religions. (2021) 12:757. doi: 10.3390/rel12090757
66. Fatima, S, Arshad, M, and Mushtaq, M. Religious coping and young adult's mental well-being during Covid-19: testing a double moderated mediation model. Arch Psychol Relig. (2022) 44:158–74. doi: 10.1177/00846724221121685
67. Schnabel, L, and Schieman, S. Religion protected mental health but constrained crisis response during crucial early days of the COVID-19 pandemic. J Sci Study Relig. (2022) 61:530–43. doi: 10.1111/jssr.12720
68. Kes, D, and Aydin, YT. The relationship of religious coping strategies and family harmony with caregiver burden for family members of patients with stroke. Brain Inj. (2020) 34:1461–6. doi: 10.1080/02699052.2020.1810317
69. Hood, RW, Hill, PC, and Williamson, WP. The psychology of religious fundamentalism. New York: Guilford Press. (2005).
70. Cetın, Z, and Ozen, B. Investigating spiritual care perceptions and religious coping methods among the relatives of terminally ill patients during the COVID-19 pandemic: the case of Turkey. BMC Palliat Care. (2024) 23:131. doi: 10.1186/s12904-024-01463-x
71. Di Tella, M, Romeo, A, Benfante, A, and Castelli, L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J Eval Clin Pract. (2020) 26:1583–7. doi: 10.1111/jep.13444
72. Huang, JZ, Han, MF, Luo, TD, Ren, AK, and Zhou, XP. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. (2020) 38:192–5. doi: 10.3760/cma.j.cn121094-20200219-00063
73. Kisely, S, Warren, N, McMahon, L, Dalais, C, Henry, I, and Siskind, D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. (2020) 369:m1642. doi: 10.1136/bmj.m1642
74. Almeida, T, Silva, S, Duarte, F, Queiroz, C, Araújo, P, Assis Neves Dantas, R, et al. Analysis of post-traumatic stress disorder in nursing professionals during the COVID-19 pandemic. Texto Contexto - Enfermagem. (2022) 31:e20220139. doi: 10.1590/1980-265X-TCE-2022-0139en
75. Cuartero-Castañer, ME, Hidalgo-Andrade, P, and Cañas-Lerma, AJ. Professional quality of life, engagement, and self-care in healthcare professionals in Ecuador during the COVID-19 pandemic. Healthcare. (2021) 9:515. doi: 10.3390/healthcare9050515
76. Inocian, EP, Cruz, JP, Saeed Alshehry, A, Alshamlani, Y, Ignacio, EH, and Tumala, RB. Professional quality of life and caring behaviours among clinical nurses during the COVID-19 pandemic. J Clin Nurs. (2021) 1–13. doi: 10.1111/jocn.15937
77. Serrão, C, Martins, V, Ribeiro, C, Maia, P, Pinho, R, Teixeira, A, et al. Professional quality of life among physicians and nurses working in Portuguese hospitals during the third wave of the COVID-19 pandemic. Front Psychol. (2022) 13:814109. doi: 10.3389/fpsyg.2022.814109
78. Ruiz-Fernández, MD, Ramos-Pichardo, JD, Ibáñez-Masero, O, Cabrera-Troya, J, Carmona-Rega, MI, and Ortega-Galán, ÁM. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J Clin Nurs. (2020) 29:4321–30. doi: 10.1111/jocn.15469
79. Trumello, C, Bramanti, SM, Ballarotto, G, Candelori, C, Cerniglia, L, Cimino, S, et al. Psychological adjustment of healthcare Workers in Italy during the COVID-19 pandemic: differences in stress, anxiety, depression, burnout, secondary trauma, and compassion satisfaction between frontline and non-frontline professionals. Int J Environ Res Public Health. (2020) 17:8358. doi: 10.3390/ijerph17228358
80. Brooks, SK, Webster, RK, Smith, LE, Woodland, L, Wessely, S, Greenberg, N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
81. Feiler, T, Vanacore, S, and Dolbier, C. COVID-19 pandemic-specific PTSD: risk and protective factors among university students. J Loss Trauma. (2023) 28:537–53. doi: 10.1080/15325024.2022.2132670
82. Carroll, T, McCormick, W, Smith, P, Isaak, S, and Currier, J. PTSD, religious coping, and interpersonal antecedents of suicidal desire among military veterans: an initial examination of moderation models. Psychol Relig Spiritual. (2019) 12:304–10. doi: 10.1037/rel0000270
83. Mesidor, JK, and Sly, K. Religious coping, general coping strategies, perceived social support, PTSD symptoms, resilience, and posttraumatic growth among survivors of the 2010 earthquake in Haiti. Mental Health Relig Cult. 22:130–43. doi: 10.1080/13674676.2019.1580254
84. Sujadi, E, Meditamar, M, Fadhli, M, Ahmad, J, Bustami, Y, and Indra, S. Posttraumatic stress disorder among sexual harassment victims: the role of social support, resilience, and religious coping. Int J Public Health Sci (IJPHS). (2023) 12:846. doi: 10.11591/ijphs.v12i2.21952
85. Bagheri-Nesami, M, Kazemi, A, Goudarzian, AH, Nasiri, F, and Davari, J. Association between religious coping and quality of working life in nurses. Iran J Psychiatry Behav Sci. (2017) 11:e4946. doi: 10.5812/ijpbs.4946
86. MohammadMehdi, S, Batool, N, and Masoud, SN. Spiritual coping strategies to Deal with job burnout among military nurses: a qualitative study. J Milit Med. (2021) 23:472–81. doi: 10.30491/JMM.23.6.472
87. Yildirim, JG, and Ertem, M. Professional quality of life and perceptions of spirituality and spiritual care among nurses: relationship and affecting factors. Perspect Psychiatr Care. (2022) 58:438–47. doi: 10.1111/ppc.12794
88. Bastani, F, Ghasemi, E, Ramezanzadeh Tabriz, E, Janani, L, and Rahmatnejad, L. The investigation of perceived stress and religious coping among female caregivers of the elderly with dementia. J Rafsanjan Univ Med Sci. (2015) 13:925–36.
89. Cohen, R, Leykin, D, Golan-Hadari, D, and Lahad, M. Exposure to traumatic events at work, posttraumatic symptoms and professional quality of life among midwives. Midwifery. (2017) 50:1–8. doi: 10.1016/j.midw.2017.03.009
91. Tirgari, B, Azizzadeh Forouzi, M, and Ebrahimpour, M. Relationship between posttraumatic stress disorder and compassion satisfaction, compassion fatigue, and burnout in Iranian psychiatric nurses. J Psychosoc Nurs Ment Health Serv. (2019) 57:39–47. doi: 10.3928/02793695-20181023-02
92. Counted, V, Pargament, K, Bechara, A, Joynt, S, and Cowden, R. Hope and well-being in vulnerable contexts during the COVID-19 pandemic: does religious coping matter? J Posit Psychol. (2020) 17:70–81. doi: 10.1080/17439760.2020.1832247
93. Snapp, M, and Hare, L. The role of spiritual care and healing in health management. Adv Mind Body Med. (2021) 35:4–8.
94. McCleary-Gaddy, A, and Miller, C. Negative religious coping as a mediator between perceived prejudice and psychological distress among African Americans: a structural equation modeling approach. Psychol Relig Spiritual. (2018) 11:257–65. doi: 10.1037/rel0000228
95. Ibrahim, MA, Isa, KQ, Haji-Idris, H-A, Nawi, S-H, Teo, YC, Abdul Rahman, H, et al. Spiritual coping with stress among emergency and critical care nurses: a cross-sectional study. Community Ment Health J. (2020) 56:287–93. doi: 10.1007/s10597-019-00486-6
96. DeRossett, T, LaVoie, DJ, and Brooks, D. Religious coping amidst a pandemic: impact on COVID-19-related anxiety. J Relig Health. (2021) 60:3161–76. doi: 10.1007/s10943-021-01385-5
97. Imran, MH, Zhai, Z, and Iqbal, M. The role of religious coping to overcome mental distress and anxiety during the COVID-19 pandemic: an integrative review. Anal Soc Issues Public Policy. (2022) 22:817–35. doi: 10.1111/asap.12327
98. Wnuk, M. The mechanisms underlying religious coping and hopelessness: role of meaning in life and affectivity. Pastor Psychol. Advance online publication. doi: 10.1007/s11089-024-01181-4
99. Norris, FH, and Riad, JK. Standardized self-report measure of civilian trauma and post traumatic stress disorder. In Editors JP. Wilson and TM Keane, Assessing psychological trauma and PTSD. New York: Guilford Publications. (1997), pp. 7–42.
100. Pargament, KI. The psychology of religion and coping: Theory, research, practice. New York: The Guilford Press. (2000).
101. Bahrami Ehsan, H. Preliminary study of validity and reliability of religious orientation scale. J Psychol Educ. (2001) 6:67–90. Retrieved from https://sid.ir/paper/55700/en
102. Ghiami, Z. An investigation about the relation of attachment styles with religious coping styles. J Psychol Educ. (2005) 35:221–33. Retrieved from https://sid.ir/paper/55656/en
Keywords: religious and spiritual coping, post-traumatic stress disorder, quality of life, nurse, COVID-19
Citation: Sanavi Shiri Z, Tavakoli P and Momennasab M (2025) Relationship between religious coping and post-traumatic stress disorder and professional quality of life of nurses working at COVID-19 wards: a descriptive correlational study. Front. Public Health. 13:1535340. doi: 10.3389/fpubh.2025.1535340
Edited by:
Carla Viegas, Instituto Politécnico de Lisboa, PortugalReviewed by:
Mohammad Ali Zakeri, Rafsanjan University of Medical Sciences, IranBenedict Francis, University of Malaya, Malaysia
Copyright © 2025 Sanavi Shiri, Tavakoli and Momennasab. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marzieh Momennasab, bW9tZW5uYXNhYkBzdW1zLmFjLmly
 Zohreh Sanavi Shiri
Zohreh Sanavi Shiri Pouran Tavakoli
Pouran Tavakoli Marzieh Momennasab
Marzieh Momennasab


